Assessing Clinical Reasoning: Identifying the GAP
MedEdPearls November 2018: What strategies might you use to address gaps in clinical reasoning?
At the end of a case presentation, you ask your learner “what’s the patient diagnosis?”, and you think to yourself “what’s the learner diagnosis?”
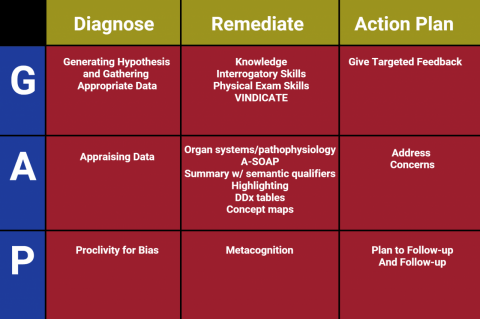
Consider the GAP in clinical reasoning. Focus on the following:
- Generating Hypothesis and Gathering Appropriate Data – identified by poor problem representation; difficulties in generating hypotheses; identifying cues and directed data gathering
- Appraising Data – identified by difficulties in building an overall picture; difficulties in prioritizing; difficulties in elaborating a management plan
- Proclivity for Bias – premature closure; availability; confirmation
Learners may have more than one deficiency. Consider the following remedial exercises:
- G– role play to demonstrate use of communication and physical examination skills; VINDICATEmnemonic to generate a broader hypothesis
- A– highlight pertinent information; develop concept maps for problems; explicitly demonstrate semantic transformation of problems
- P – discuss justification of main hypothesis and generate alternative hypotheses
References
- Audétat MC, Laurin S, Dory V, Charlin B, Nendaz MR. Diagnosis and management of clinical reasoning difficulties: Part II. Clinical reasoning difficulties: Management and remediation strategies.Med Teach. 2017 Aug;39(8):797-801. doi: 10.1080/0142159X.2017.1331034. Epub 2017 Jun 7.
- Weinstein A, Gupta S, Pinto-Powell R, et al. Diagnosing and remediating clinical reasoning difficulties: a faculty development workshop. MedEdPORTAL. 2017; 13:10650. https://doi.org/10.15766/mep_2374-8265.10650
About the MedEdPearls Author
The MedEdPearls are a collaborative, peer-reviewed, monthly brief intended to provide practical tips and strategies for medical and health professions educators to enhance teaching and learning.

Shanu Gupta
MD
- Associate Professor of Internal Medicine, University of South Florida Morsani College of Medicine
- Program Director, Academy of Distinguished Educators, University of South Florida Morsani College of Medicine
- Jean Bailey, PhD – Virginia Commonwealth University School of Medicine
- Carrie Bowler, EdD, MS, MLSCM (ASCP) – Mayo Clinic School of Continuous Professional Development
- Kristina Dzara, PhD, MMSc (Educators ’16; Assessment ’16; HCE 2.0 ’17) – Saint Louis University School of Medicine
- Shanu Gupta, MD, SFHM – University of South Florida Morsani College of Medicine and Tampa General Hospital
- Jennifer Hillyer, PhD – Northeast Ohio Medical University
- Larry Hurtubise, PhD, MA (HCE 2.0 '16) – The Ohio State University
- Anna Lama, EdD, MA – West Virginia University School of Medicine
- Machelle Linsenmeyer, EdD, NAOME (Assessment ’07) – West Virginia School of Osteopathic Medicine
- Skye McKennon, PharmD, BCPS, ACSM-GEI – Washington State University Elson S. Floyd College of Medicine
- Rachel Moquin, EdD, MA – Washington University School of Medicine
- Stacey Pylman, PhD – Michigan State University College of Human Medicine
- Leah Sheridan, PhD – Northeast Ohio Medical University
- Lonika Sood, MBBS, MHPE – Washington State University Elson S. Floyd College of Medicine
- Mark Terrell, EdD – Lake Erie College of Osteopathic Medicine
- Stacey Wahl, PhD – Virginia Commonwealth University School of Medicine
Harvard Macy Institute
Harvard Macy Institute
The Harvard Macy Institute educates, connects, and serves health care leaders around the globe by providing advanced faculty development programs, thought leadership, and impactful networking opportunities.
6 Programs